Using tissue-like bioengineered hydrogels, patient tumours can be preserved for up to 10 days, facilitating personalised screening of cancer drugs to enhance treatment effectiveness
In a breakthrough for personalised oncology, scientists from the National University of Singapore (NUS) and the National Cancer Centre Singapore (NCCS), have developed and demonstrated a novel platform that can significantly reduce the time needed to determine the efficacy of anti-cancer drugs. In this first-of-its-kind technology, patient tumours resected from surgery can now be grown and better preserved ex vivo (outside of the body) compared to standard approaches, potentially accelerating the process for drug screening and testing for individual cancer patients.
Tumours are highly complex tissues comprising not just the rapidly proliferating cancer cells, but also a dynamic array of supporting cells such as immune cells. The nature and composition of the different types of cells within each tumour can vary widely, even amongst patients with similar backgrounds, demographics, and lifestyles. Hence, two patients with the same cancer may respond differently to the same drug given. There is no guarantee that the drug or drugs administered based on cohort response, will work for a specific patient.
Assistant Professor Eliza Fong, co-lead of the research study, who is from the Department of Biomedical Engineering at the NUS College of Design and Engineering and the N.1 Institute for Health, explained, “Tumours are not just made up of cancer cells. The various cells in a tumour can be likened to the different pieces in a chess set. The king, akin to cancer cells, is protected and supported by other pieces or cell types present in the tumour. You can think of these supporting cells as the pawns, rooks, bishops and knights. Many drugs now target these supporting cells to eliminate cancer cells.”
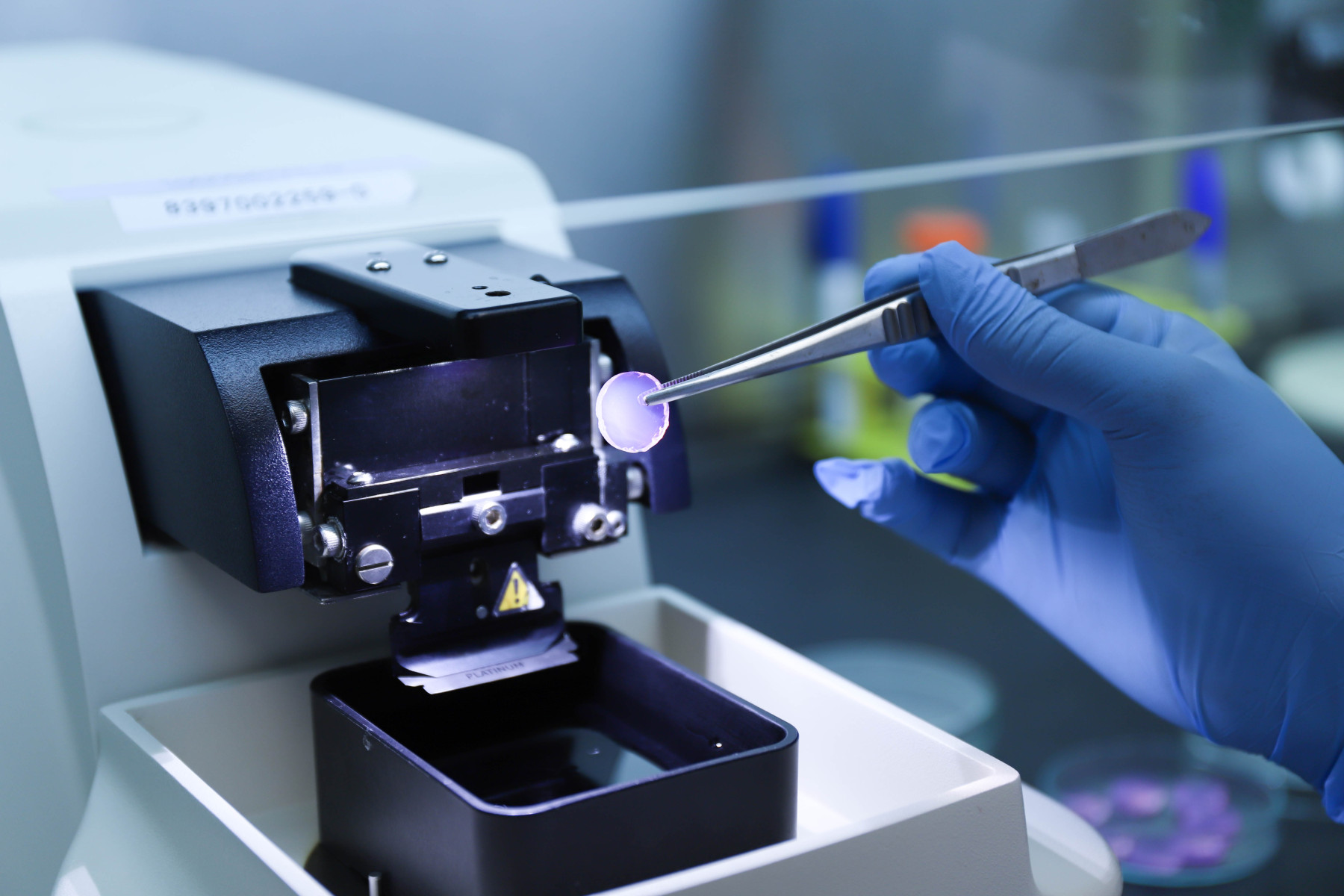
The breakthrough in this study, she added, is in the use of tissue-like, bioengineered hydrogels to keep the patient’s tumour alive even after it has been removed from the body. Assistant Professor Fong explained, “What we have done here, is to develop a materials-based platform that allows fragments of the tumour – with all of the various chess pieces – to be preserved outside the body for up to 10 days. This is much longer than what is currently possible. Employing traditional methods, it is only possible to maintain tumours for one to two days outside the body, using the same kind of plastic material that can be found in cookware. This new bioengineering approach that the team has developed opens up unprecedented opportunities for the efficient and accurate testing of anti-cancer drugs on the patient’s tumor, including immunotherapies, for individual cancer patients. These tumour fragments can now serve as true ‘patient avatars’ for personalised oncology.”
The results of the study were published in the journal Biomaterials on 20 January 2024.
A novel hydrogel-based platform to preserve patient-derived tumour slices
The study revealed several key findings. First, tumour fragments cultured in the platform were better preserved in terms of viability and morphology as compared to standard methods over time. The ability to maintain tumour fragments alive for up to 10 days allows for more drug testing and screening to be performed.
Second, through advanced characterisation including sequencing at the single-cell level, the researchers robustly demonstrated that all of the various chess pieces in the original tumour – including cancer cells, immune cells and fibroblasts – were also present in the cultured tumour fragments. The retention of the various pieces in the cultured tumour allows these ‘patient avatars’ to better depict the effects of drugs on cancer cells.
Furthermore, the study also showed the utility of these ‘patient avatars’ for testing immune checkpoint inhibitors, a type of immunotherapy, in a co-clinical trial. These ‘patient avatars’ could accurately predict the drug response of head and neck cancer patients from which the tumours were resected and cultured. Hence, the platform may help to guide clinicians in selecting patients to prescribe these immune checkpoint inhibitors, while reducing the possibility of giving the drug to patients whose tumours are least likely to respond to treatment.
Advantages of the new hydrogel-based platform
The use of this platform in cancer research has several advantages over traditional cell culture models. By preserving the tumour microenvironment and maintaining the heterogeneity of the cells within the patient’s tumour, it offers a more accurate representation of the complex interactions between the different cell types in the tumour. This breakthrough allows researchers to study the effects of drugs and therapies in a more realistic setting, potentially leading to more effective treatment strategies.
Professor Gopal Iyer, co-lead of this study, who is a Clinician Scientist and Head of the Department of Head and Neck Surgery at the National Cancer Centre Singapore, said, “As an oncologist and scientist, my goal is to treat patients better and that means giving the right drug to the right patient at the right time, and in the right combination. It takes at least six months to tell if a cancer therapy is working and even blockbuster immunotherapy drugs – the best pharmacological option currently available to patients with advanced disease – have a success rate of around 20 per cent. This platform allows us to test drugs in a more realistic setting with the goal of improving their efficacy. With this, we hope to alleviate some of the uncertainty and anxiety that can be a part of a patient’s experience when they undergo cancer treatment.”
Advancing the field of personalised medicine
The findings from this study have significant implications for personalised medicine and the development of targeted therapies. By studying the response of individual tumours to specific treatments, researchers can identify biomarkers and predictive factors that can guide treatment decisions. This personalised approach has the potential to revolutionise cancer treatment and improve patient outcomes.
The team is working on a larger-scale clinical trial to validate this new tissue-like, bioengineered material. They also hope to build a local repository of tumours for Singapore and the region that can be used for more comprehensive drug testing and pre-screening. “Cancer treatment can be a challenging and uncertain journey. But with innovations in biomaterials and personalised oncology, and strong collaborations with clinicians, we can accelerate the time taken to test and optimise drugs for individual patients in the Singapore context and beyond,” said Assistant Professor Fong.